In the Labour and Delivery (L&D) room, we celebrate when the baby is born. But sometimes, the crisis only begins after that.
The mother goes pale, her eyes fluttering. Blood loss picks up. The uterus doesn’t contract. Trays are passed, and IV lines are opened. The midwife kneels to perform bimanual compression, pressing against a uterus that’s not responding. As the vitals on the monitor shift, the shock index becomes a dangerous 1…and keeps rising.
This is a scene that plays out more often than we’d like.
In Malaysia, maternal deaths climbed to 68.2 per 100,000 live births during the pandemic, and although official figures dropped back to 25.7 in 2023, the risk remains urgent. Postpartum haemorrhage (PPH) is still one of the leading causes of maternal death in the country. It can go from stable to fatal in under an hour. And when it does, everyone in the medical team needs to be prepared. In many cases, the person most likely to respond first, especially in district or semi-urban hospitals, is the midwife.
They are the emergency anchors in the L&D room. As they monitor all the stages of labour, catching the signs that others might miss, they are often the first to diagnose emergencies and alert the team. In those first few minutes, the outcome hinges on their ability to stay calm, act quickly, and make confident clinical decisions.

Obstetric emergencies are unpredictable. Some midwives may not encounter shoulder dystocia or uterine inversion for months. But when it happens, the team needs someone whose response is automatic.
Without regular, structured training, even experienced clinicians can hesitate. Protocols blur. Sequences get muddled. And in a field where every minute matters, delays can mean the difference between recovery and tragedy.
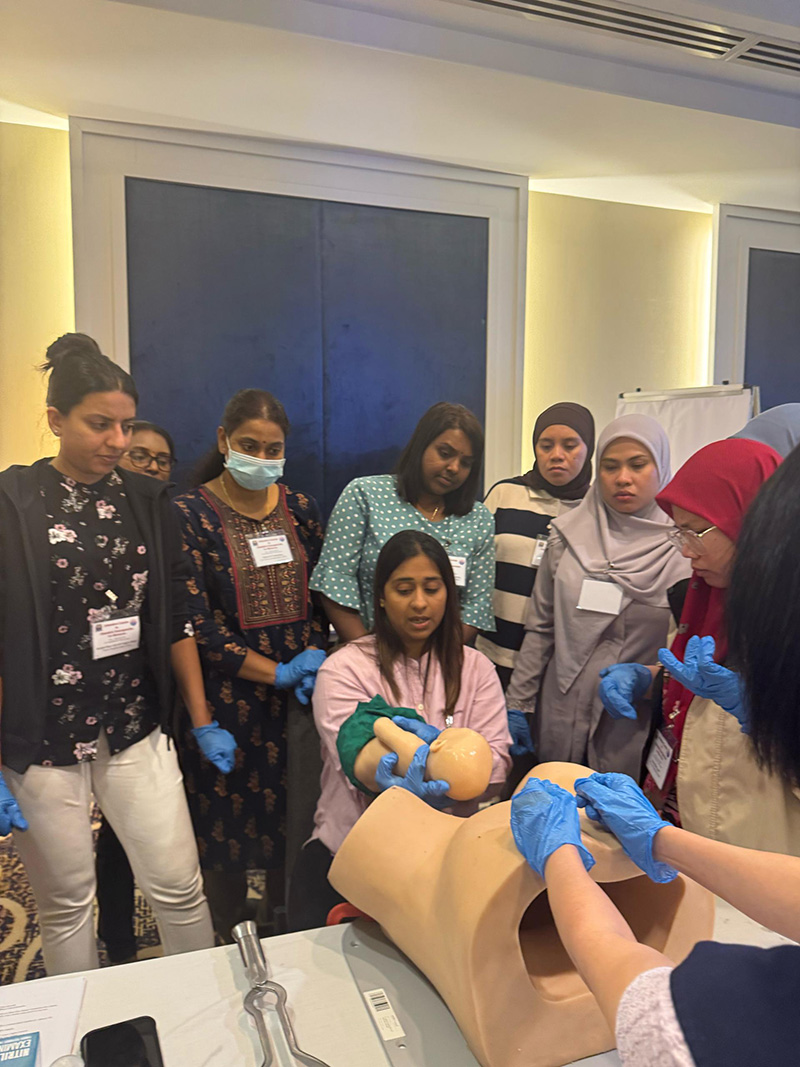
The Intensive Course in Obstetric Emergencies (ICOE) was developed by the Obstetrical and Gynaecological Society of Malaysia to address exactly this. The programme is designed especially for midwives to sharpen reflexes, reinforce clinical reasoning, and create muscle memory through simulation-based, scenario-driven training.
At the 31st ICOE in Kuala Lumpur this April, the training began before the simulations. Midwives underwent pre-course assessments to benchmark their skills. Over two days, they rotated through six breakout rooms, each one replicating a high-risk emergency from the labour ward or postpartum unit.
They practised maternal resuscitation — airway manoeuvres, chest compressions, and fluid replacement — tailored for pregnancy. PPH drills covered everything from uterotonics to bimanual compression and managing uterine inversion. Labour ward simulations focused on breech births, shoulder dystocia, and cord prolapse. Medical scenarios like eclampsia, sepsis, and hypertensive crises were also covered, alongside sharpening non-technical skills like Cardiotocography (CTG) interpretation, partograph use, and structured handovers using the ISBAR protocol (Identify, Situation, Background, Assessment, and Recommendation).
Every 30 minutes, teams rotated to a new challenge. Sessions were short, intense, and immediately followed by instructor feedback and group debriefs. The faculty included senior midwives and obstetricians trained in adult learning and simulation methodology.
By the final day, participants faced post-course skill assessments, tracking progress in everything from CPR to estimation of blood loss.

ICOE’s training is designed to build confidence to act early and escalate fast. In the real world, the ward might be understaffed or stretched, but a well-trained midwife is never unprepared.
And the effects of the training always ripple outward. One confident midwife in the delivery suite often sets the tone for the rest of the team. Midwives trained in ICOE return with more than skill; they return to their healthcare settings with a sense of urgency, understanding how fast things can go wrong, and how quickly things can be made right when a team is prepared.
And they go back to lead. Whether it’s Internal drills, peer coaching, or even advocating at large for safety protocols in their own hospitals.



