Maternal health outcomes in Malaysia have improved steadily over the past decades, with maternal mortality ratios falling from over 40 per 100,000 live births in the 1990s to under 30 today. Yet, obstetric emergencies remain a stubborn challenge. They may be rare, but when they strike, they are catastrophic, demanding immediate, coordinated action to prevent maternal and neonatal deaths.
Why Simulation Matters in Obstetric Emergencies
Traditional obstetrics training often relies on didactic teaching and supervised exposure during clinical rotations. While this builds knowledge, it does not fully prepare clinicians for the intensity of real-life emergencies.
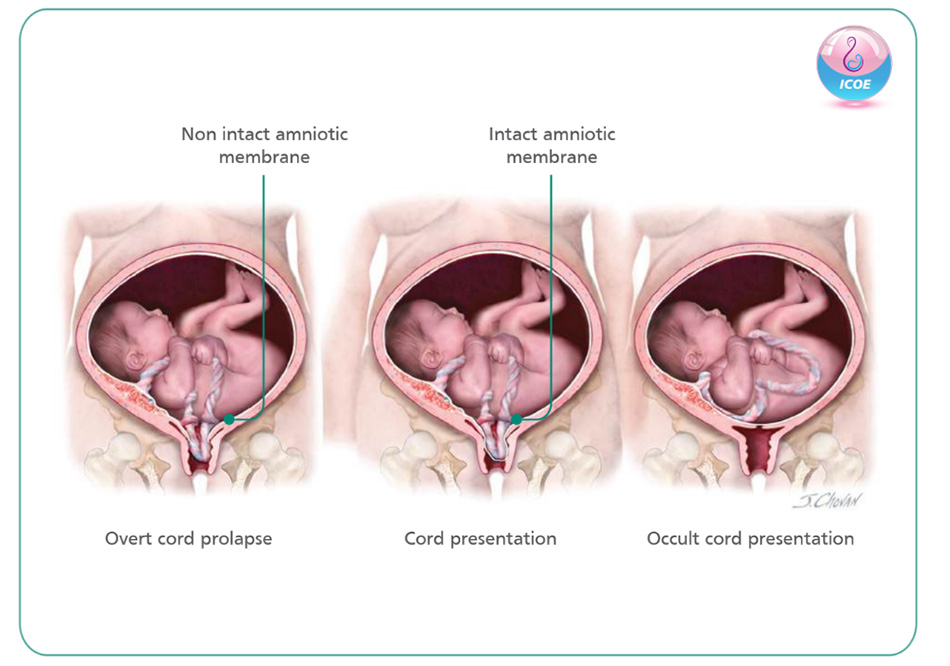
Caesarean deliveries are the most common surgery globally. However, rare but potentially catastrophic events like cord prolapse or uterine rupture can throw even experienced teams off balance.
Simulation training fills this gap. Evidence shows that teams who rehearse obstetric emergencies in realistic scenarios achieve faster decision-to-delivery times, communicate more effectively, and make fewer errors. Programmes by the Royal College of Obstetricians and Gynaecologists (RCOG) and the American College of Obstetricians and Gynaecologists (ACOG) have demonstrated measurable improvements in outcomes. Adapting these approaches to local realities is vital to strengthening emergency preparedness in Malaysian hospitals.
The Malaysian Context
Obstetric practice here is diverse. Tertiary centres in cities may see high case volumes and complex pathologies, while district hospitals often operate with limited staff and equipment. For junior obstetricians posted outside urban hubs, exposure to high-risk emergencies can be infrequent, leading to skill and confidence gaps when crises do arise.
Simulation allows teams to practice not only technical steps, but also communication strategies that flatten hierarchies and improve response speed.
What Simulation Teaches Beyond Technique
The true value of simulation lies in its holistic approach. Emergencies are not managed by obstetricians alone; they demand coordinated teamwork across multiple disciplines. Through scenario-based training, participants practise:
- Closed-loop communication to ensure instructions are heard, acknowledged, and acted upon.
- Role clarity, with each member, whether anaesthetist, scrub nurse, or lead surgeon, knowing their responsibilities.
- Surgical safety checklist to ensure no critical steps are missed.
- Stress management, building resilience so that cognitive and technical skills hold steady even under extreme pressure.

ICOE’s Role in Strengthening Emergency Preparedness
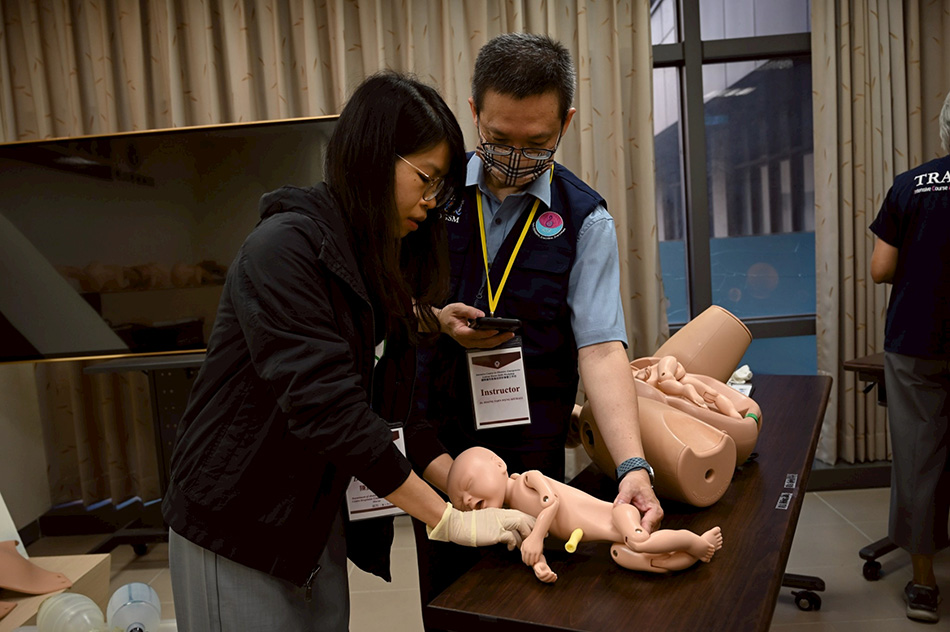
ICOE uses simulation as the cornerstone of training. An Emergency caesarean delivery course combines hands-on drills, multidisciplinary participation, and scenario-based challenges with high-fidelity training equipment designed to mirror Malaysian hospital realities. Participants consistently highlight how rehearsing under pressure reshaped their confidence and sharpened their teamwork.
This approach aligns with the Ministry of Health’s ongoing commitment to reducing maternal morbidity and mortality by investing in workforce readiness. By embedding simulation into professional development, ICOE supports a culture of safety that extends beyond individuals to entire hospital systems.


