In obstetric practice, you put in years of training preparing for emergencies, until one day your worst nightmare comes true. You’re faced with an emergency that sends the entire team into panic.
But when a patient presents with a prolapsed umbilical cord, letting the panic get in the way is simply not an option. How quickly you respond can mean the difference between a healthy birth and irreversible harm.
Why It Matters
Umbilical cord prolapse (UCP) occurs in about 0.1% to 0.6% of all births. It’s relatively uncommon, but when it happens, fetal hypoxia can set in within minutes due to cord compression. The window for action is narrow, ideally, delivery within 10–20 minutes of diagnosis.
Globally, hospitals that have established clear response protocols have reported dramatic reductions in neonatal morbidity and mortality. But what about Malaysia?
While our national neonatal mortality rate sits at 4.3 per 1,000 live births (as of 2023), the specific impact of emergencies like UCP is not widely reported in national data. However, based on tertiary hospital audits and clinical experience, the urgency is no less real.
What Causes Cord Prolapse?
UCP is typically linked to one or more risk factors. While it can occur spontaneously, several scenarios significantly raise the odds:
Patient-related risk factors:
- Malpresentation (breech, transverse, unstable lie)
- Prematurity (less than 37 weeks)
- Polyhydramnios
- Multiple pregnancies (especially second set of twins)
- Grand multiparity
Iatrogenic factors:
- Amniotomy with an unengaged head
- Manipulative procedures (e.g., internal rotation)
- Induction or augmentation with an unstable lie
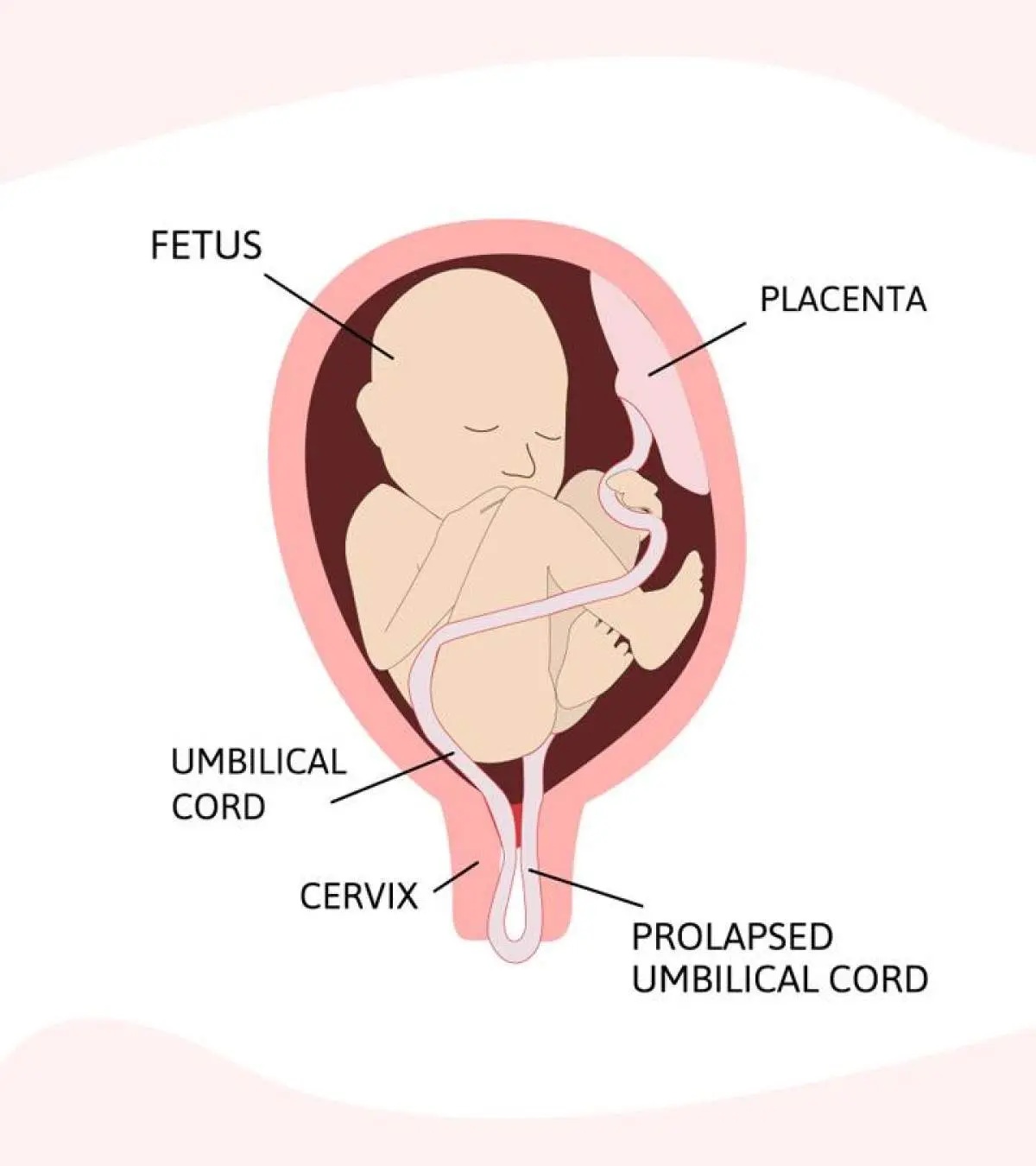
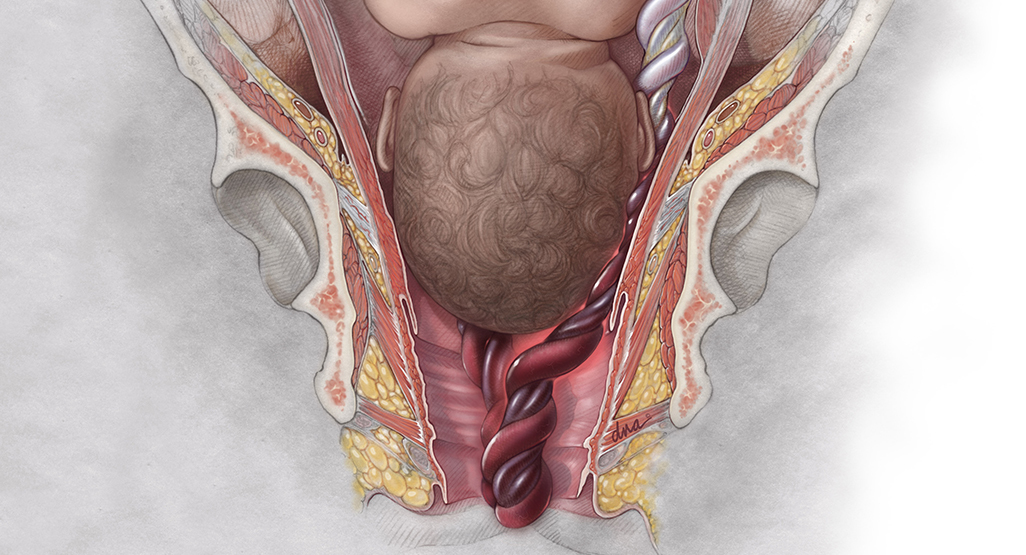
Recognising Cord Prolapse
The hallmark of cord prolapse is sudden, prolonged fetal bradycardia or recurrent variable decelerations—a recognisable red flag on CTG. Clinically, it may present as:
- Overt prolapse: Cord is felt or seen in the vagina after membrane rupture.
- Occult prolapse: Cord lies beside the presenting part; no visible cord, but fetal compromise is evident.
Vigilance during labour monitoring is essential, particularly when any risk factors are present. In several Malaysian hospitals, it’s now standard to alert theatre teams early when high-risk profiles are identified, even before labour is established.
What To Do When It Happens
Once UCP is diagnosed, time is critical. Management steps include:
- Call for immediate help—obstetrics, anaesthesia, paediatrics, and OT staff.
- Relieve pressure on the cord:
- Manually elevate the presenting part.
- Position the patient in knee–chest or Trendelenburg position.
- Consider bladder filling with 500–750 mL saline via a Foley catheter.
- Avoid handling the cord to prevent vasospasm.
- Prepare for rapid delivery:
- Emergency C-section is the standard of care unless vaginal delivery is imminent and safe.
- Aim for a decision-to-delivery interval (DDI) <30 minutes, ideally <15.
How Simulation Changes the Game
Structured training isn’t just theory. It changes how teams respond in real emergencies.
In a 2022 study published in Contemporary OB/GYN, simulation training improved DDI from 25 minutes to 14.5 minutes. More importantly, post-training cases saw no neonates with Apgar scores <7 at five minutes.
Multiple other studies have shown similar results, like the one from Sun Yat-sen University in China (2024) that showed team-based simulation training for umbilical cord prolapse significantly improved clinical outcomes. After participating in regular drills, healthcare teams responded faster, communicated more effectively, and were able to reduce the time from diagnosis to delivery.
Closer to home, the Intensive Course in Obstetric Emergencies (ICOE), a flagship programme by the Obstetrical and Gynaecological Society of Malaysia, routinely incorporates cord prolapse drills. Malaysia’s updated Perinatal Care Manual (4th edition, 2023) also underscores proactive identification and management of obstetric emergencies, including cord prolapse

“Some things are more worthwhile than monetary gains,” reflected Dr. Patricia, a long-term ICOE trainer, after a successful team simulation led to real-world success weeks later. “One group stood out for creatively using materials from their local setting to simulate a cord prolapse drill, showing strong leadership, teamwork, and a clear understanding of the task. That’s how ICOE prepares doctors.”
Lessons from the Field
Across hospitals in Malaysia—from urban teaching hospitals to rural district centres—teams who have trained together report:
- Increased confidence in high-pressure scenarios
- Faster mobilisation to operation theatre
- Improved neonatal outcomes
- Better documentation of events, interventions, and outcomes
Moving Forward: From Protocol to Practice
So, how do we strengthen Malaysia’s readiness for UCP?
- Embed UCP response drills into every labour ward’s standard operating procedure
- Invest in training with ICOE or similar simulation-based training
- Use incident reviews and debriefs to refine response time and coordination
- Integrate cord prolapse algorithms into emergency trolleys, charts, and CME
We’ve made strides in improving maternal health and reducing perinatal deaths. But cord prolapse remains a stark reminder that preparedness must be proactive, not reactive.
While it may only affect a small fraction of births, but for each baby and mother, it’s a once-in-a-lifetime event. How we respond, how quickly, how cohesively, can change the story.



